Cobalt Allergy – Symptoms, Causes, Diagnosis & Treatment
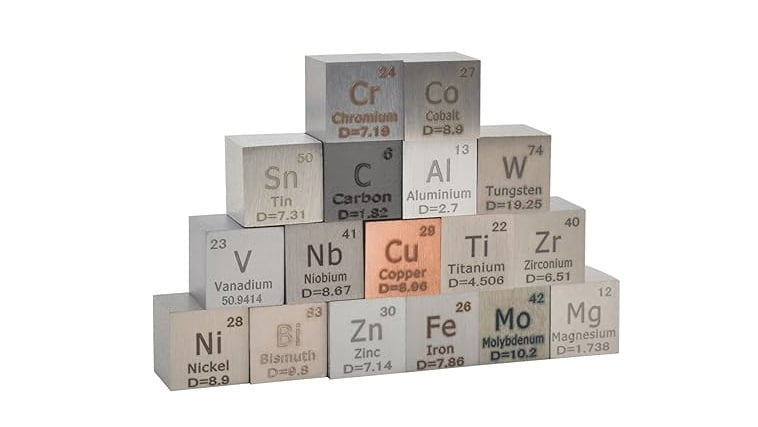
Cobalt allergy is a type of metal allergy characterized by an adverse immune response to cobalt, a naturally occurring element found in many everyday items such as jewelry, dental implants, and orthopedic implants. While cobalt is widely used in various industries due to its durability and magnetic properties, some individuals may develop allergic reactions upon exposure. In this comprehensive overview, we will explore the symptoms, causes, diagnosis, and treatment of cobalt allergy.
Symptoms of Cobalt Allergy:
Symptoms of cobalt allergy can vary depending on the individual’s sensitivity and the extent of exposure. Common symptoms may include:
- Skin Rash:
- Redness, itching, and inflammation at the site of contact with cobalt-containing materials, such as jewelry or clothing accessories.
- The rash may be localized or spread to other areas of the body.
- Dermatitis:
- Contact dermatitis, characterized by dry, scaly, or blistering skin, particularly in areas of prolonged contact with cobalt.
- Symptoms may resemble eczema or other types of allergic skin reactions.
- Swelling:
- Swelling (edema) of the skin, particularly around the site of contact.
- In severe cases, swelling may extend beyond the immediate area of contact and affect nearby tissues.
- Hives (Urticaria):
- Respiratory Symptoms:
- In rare cases of systemic exposure or inhalation of cobalt dust, individuals may experience respiratory symptoms such as wheezing, coughing, or shortness of breath.
- Severe respiratory reactions, including asthma exacerbation or anaphylaxis, are uncommon but can occur in highly sensitive individuals.
- Systemic Symptoms:
Causes of Cobalt Allergy:
Cobalt allergy occurs when the body’s immune system mistakenly identifies cobalt ions as harmful substances and mounts an immune response to eliminate them. The exact mechanisms underlying cobalt allergy are not fully understood, but several factors may contribute to its development:
- Sensitization:
- Prolonged or repeated exposure to cobalt-containing materials can sensitize the immune system, leading to the production of specific antibodies (IgE or IgG) against cobalt ions.
- Genetic Predisposition:
- Genetic factors may play a role in determining an individual’s susceptibility to metal allergies, including cobalt allergy.
- Occupational Exposure:
- Certain occupations, such as metalworking, jewelry making, and dental work, involve regular exposure to cobalt-containing materials, increasing the risk of sensitization and allergy development.
- Cross-Reactivity:
- Individuals sensitized to other metals, such as nickel or chromium, may also exhibit cross-reactivity to cobalt due to structural similarities between metal ions.
- Implant Materials:
- Orthopedic implants, joint replacements, and dental prosthetics may contain cobalt as an alloying element, potentially triggering allergic reactions in sensitive individuals.
- Environmental Exposure:
- Environmental sources of cobalt, such as cobalt dust or fumes from industrial processes, may contribute to sensitization and allergy development, particularly in occupational settings.
Diagnosis of Cobalt Allergy:
Diagnosing cobalt allergy typically involves a combination of medical history, clinical evaluation, and specialized tests to assess immune reactivity. Key steps in the diagnostic process include:
- Medical History:
- The healthcare provider will inquire about the patient’s symptoms, occupation, hobbies, and potential sources of cobalt exposure, including recent use of jewelry, dental work, or occupational activities.
- Physical Examination:
- A thorough examination of the skin, particularly areas of suspected contact dermatitis or allergic reactions, may reveal characteristic signs of this allergy, such as rash or inflammation.
- Patch Testing:
- Patch testing is the gold standard for diagnosing metal allergies, including cobalt allergy. During patch testing, small amounts of cobalt or cobalt-containing substances are applied to the skin (usually on the back) and covered with adhesive patches. After 48 hours, the patches are removed, and the skin is evaluated for signs of allergic reaction.
- Positive patch test reactions, characterized by redness, swelling, or blistering at the site of cobalt exposure, indicate sensitization and confirm the diagnosis of cobalt allergy.
- Blood Tests:
- Specific IgE or IgG blood tests may be performed to detect antibodies against cobalt ions in the bloodstream. However, these tests are less commonly used than patch testing and may have limited sensitivity and specificity for diagnosing metal allergies.
- Elimination Diet:
- In cases of suspected systemic cobalt allergy due to dietary exposure, an elimination diet may be recommended to identify and avoid cobalt-containing foods or supplements.
Treatment of Cobalt Allergy:
The management of cobalt allergy focuses on symptom relief, avoidance of cobalt exposure, and, in some cases, desensitization or immunomodulatory therapy. Treatment strategies may include:
- Topical Therapies:
- Emollients, moisturizers, or topical corticosteroids may be prescribed to alleviate symptoms of contact dermatitis and reduce skin inflammation.
- Avoidance of Cobalt Exposure:
- Identifying and avoiding sources of cobalt exposure, such as certain types of jewelry, clothing accessories, occupational materials, and dental products, is crucial for preventing allergic reactions.
- Substitution of Materials:
- In cases where cobalt-containing materials cannot be avoided, substituting non-allergenic materials or coatings may help reduce the risk of allergic reactions.
- Oral Antihistamines:
- Oral antihistamines, such as loratadine or cetirizine, may be used to relieve itching and hives associated with cobalt allergy.
- Systemic Corticosteroids:
- In severe cases of allergic dermatitis or systemic symptoms, short-term systemic corticosteroids may be prescribed to suppress inflammation and immune responses.
- Immunotherapy:
- Allergen immunotherapy, also known as desensitization or hyposensitization, involves gradually exposing the immune system to increasing doses of cobalt to induce tolerance and reduce allergic reactions. However, this approach is still experimental and not widely available for this allergy.
- Emergency Treatment:
- In rare cases of severe allergic reactions, such as anaphylaxis, immediate medical attention and treatment with epinephrine (adrenaline) may be necessary to reverse life-threatening symptoms.
Prevention Strategies:
Preventing cobalt allergy involves minimizing exposure to cobalt-containing materials and implementing preventive measures to reduce the risk of sensitization and allergic reactions. Key prevention strategies include:
- Avoidance of Known Triggers:
- Identifying and avoiding sources of cobalt exposure, including jewelry, clothing accessories, occupational materials, and dental products, is essential for individuals with this allergy.
- Selection of Hypoallergenic Materials:
- Choosing jewelry, clothing accessories, and personal care products made from hypoallergenic materials, such as titanium, surgical-grade stainless steel, or nickel-free alloys, can help reduce the risk of allergic reactions.
- Protective Measures:
- Wearing protective gloves, clothing, or barriers (e.g., tape or bandages) to minimize skin contact with cobalt-containing materials during occupational activities or hobbies.
- Regular Skin Care:
- Practicing good skincare habits, including gentle cleansing, moisturizing, and avoiding harsh or irritating substances, can help maintain skin barrier function and reduce the risk of allergic dermatitis.
- Occupational Safety Measures:
- Implementing workplace safety protocols, such as proper ventilation, personal protective equipment (PPE), and engineering controls, can minimize occupational exposure to cobalt dust or fumes in industrial settings.
Conclusion:
Cobalt allergy is an immune-mediated hypersensitivity reaction to cobalt, a common metal found in various consumer products and industrial materials. While cobalt allergy is relatively rare, it can cause significant discomfort and impairment in affected individuals. Recognition of symptoms, accurate diagnosis through patch testing, and implementation of preventive measures are essential for managing cobalt allergy and reducing the risk of allergic reactions. Collaboration between patients, healthcare providers, and occupational safety professionals is critical for effective management and prevention of this allergy in both occupational and non-occupational settings. Ongoing research efforts aimed at understanding the underlying mechanisms of cobalt allergy and developing targeted therapies may further improve outcomes for individuals with this condition.
Share this article
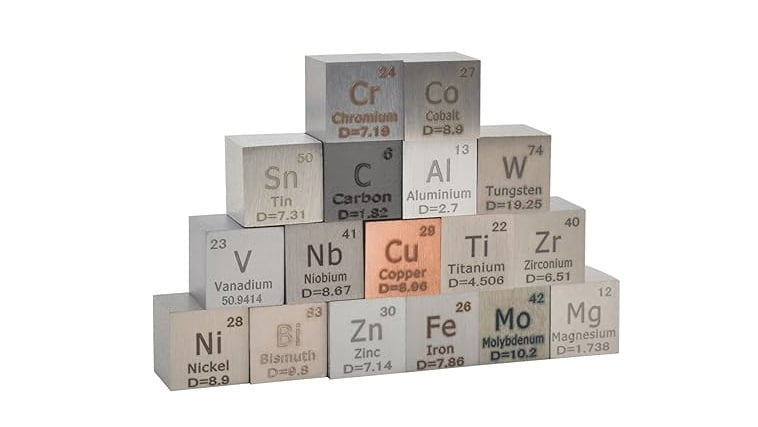
Cobalt allergy is a type of metal allergy characterized by an adverse immune response to cobalt, a naturally occurring element found in many everyday items such as jewelry, dental implants, and orthopedic implants. While cobalt is widely used in various industries due to its durability and magnetic properties, some individuals may develop allergic reactions upon exposure. In this comprehensive overview, we will explore the symptoms, causes, diagnosis, and treatment of cobalt allergy.
Symptoms of Cobalt Allergy:
Symptoms of cobalt allergy can vary depending on the individual’s sensitivity and the extent of exposure. Common symptoms may include:
- Skin Rash:
- Redness, itching, and inflammation at the site of contact with cobalt-containing materials, such as jewelry or clothing accessories.
- The rash may be localized or spread to other areas of the body.
- Dermatitis:
- Contact dermatitis, characterized by dry, scaly, or blistering skin, particularly in areas of prolonged contact with cobalt.
- Symptoms may resemble eczema or other types of allergic skin reactions.
- Swelling:
- Swelling (edema) of the skin, particularly around the site of contact.
- In severe cases, swelling may extend beyond the immediate area of contact and affect nearby tissues.
- Hives (Urticaria):
- Respiratory Symptoms:
- In rare cases of systemic exposure or inhalation of cobalt dust, individuals may experience respiratory symptoms such as wheezing, coughing, or shortness of breath.
- Severe respiratory reactions, including asthma exacerbation or anaphylaxis, are uncommon but can occur in highly sensitive individuals.
- Systemic Symptoms:
Causes of Cobalt Allergy:
Cobalt allergy occurs when the body’s immune system mistakenly identifies cobalt ions as harmful substances and mounts an immune response to eliminate them. The exact mechanisms underlying cobalt allergy are not fully understood, but several factors may contribute to its development:
- Sensitization:
- Prolonged or repeated exposure to cobalt-containing materials can sensitize the immune system, leading to the production of specific antibodies (IgE or IgG) against cobalt ions.
- Genetic Predisposition:
- Genetic factors may play a role in determining an individual’s susceptibility to metal allergies, including cobalt allergy.
- Occupational Exposure:
- Certain occupations, such as metalworking, jewelry making, and dental work, involve regular exposure to cobalt-containing materials, increasing the risk of sensitization and allergy development.
- Cross-Reactivity:
- Individuals sensitized to other metals, such as nickel or chromium, may also exhibit cross-reactivity to cobalt due to structural similarities between metal ions.
- Implant Materials:
- Orthopedic implants, joint replacements, and dental prosthetics may contain cobalt as an alloying element, potentially triggering allergic reactions in sensitive individuals.
- Environmental Exposure:
- Environmental sources of cobalt, such as cobalt dust or fumes from industrial processes, may contribute to sensitization and allergy development, particularly in occupational settings.
Diagnosis of Cobalt Allergy:
Diagnosing cobalt allergy typically involves a combination of medical history, clinical evaluation, and specialized tests to assess immune reactivity. Key steps in the diagnostic process include:
- Medical History:
- The healthcare provider will inquire about the patient’s symptoms, occupation, hobbies, and potential sources of cobalt exposure, including recent use of jewelry, dental work, or occupational activities.
- Physical Examination:
- A thorough examination of the skin, particularly areas of suspected contact dermatitis or allergic reactions, may reveal characteristic signs of this allergy, such as rash or inflammation.
- Patch Testing:
- Patch testing is the gold standard for diagnosing metal allergies, including cobalt allergy. During patch testing, small amounts of cobalt or cobalt-containing substances are applied to the skin (usually on the back) and covered with adhesive patches. After 48 hours, the patches are removed, and the skin is evaluated for signs of allergic reaction.
- Positive patch test reactions, characterized by redness, swelling, or blistering at the site of cobalt exposure, indicate sensitization and confirm the diagnosis of cobalt allergy.
- Blood Tests:
- Specific IgE or IgG blood tests may be performed to detect antibodies against cobalt ions in the bloodstream. However, these tests are less commonly used than patch testing and may have limited sensitivity and specificity for diagnosing metal allergies.
- Elimination Diet:
- In cases of suspected systemic cobalt allergy due to dietary exposure, an elimination diet may be recommended to identify and avoid cobalt-containing foods or supplements.
Treatment of Cobalt Allergy:
The management of cobalt allergy focuses on symptom relief, avoidance of cobalt exposure, and, in some cases, desensitization or immunomodulatory therapy. Treatment strategies may include:
- Topical Therapies:
- Emollients, moisturizers, or topical corticosteroids may be prescribed to alleviate symptoms of contact dermatitis and reduce skin inflammation.
- Avoidance of Cobalt Exposure:
- Identifying and avoiding sources of cobalt exposure, such as certain types of jewelry, clothing accessories, occupational materials, and dental products, is crucial for preventing allergic reactions.
- Substitution of Materials:
- In cases where cobalt-containing materials cannot be avoided, substituting non-allergenic materials or coatings may help reduce the risk of allergic reactions.
- Oral Antihistamines:
- Oral antihistamines, such as loratadine or cetirizine, may be used to relieve itching and hives associated with cobalt allergy.
- Systemic Corticosteroids:
- In severe cases of allergic dermatitis or systemic symptoms, short-term systemic corticosteroids may be prescribed to suppress inflammation and immune responses.
- Immunotherapy:
- Allergen immunotherapy, also known as desensitization or hyposensitization, involves gradually exposing the immune system to increasing doses of cobalt to induce tolerance and reduce allergic reactions. However, this approach is still experimental and not widely available for this allergy.
- Emergency Treatment:
- In rare cases of severe allergic reactions, such as anaphylaxis, immediate medical attention and treatment with epinephrine (adrenaline) may be necessary to reverse life-threatening symptoms.
Prevention Strategies:
Preventing cobalt allergy involves minimizing exposure to cobalt-containing materials and implementing preventive measures to reduce the risk of sensitization and allergic reactions. Key prevention strategies include:
- Avoidance of Known Triggers:
- Identifying and avoiding sources of cobalt exposure, including jewelry, clothing accessories, occupational materials, and dental products, is essential for individuals with this allergy.
- Selection of Hypoallergenic Materials:
- Choosing jewelry, clothing accessories, and personal care products made from hypoallergenic materials, such as titanium, surgical-grade stainless steel, or nickel-free alloys, can help reduce the risk of allergic reactions.
- Protective Measures:
- Wearing protective gloves, clothing, or barriers (e.g., tape or bandages) to minimize skin contact with cobalt-containing materials during occupational activities or hobbies.
- Regular Skin Care:
- Practicing good skincare habits, including gentle cleansing, moisturizing, and avoiding harsh or irritating substances, can help maintain skin barrier function and reduce the risk of allergic dermatitis.
- Occupational Safety Measures:
- Implementing workplace safety protocols, such as proper ventilation, personal protective equipment (PPE), and engineering controls, can minimize occupational exposure to cobalt dust or fumes in industrial settings.
Conclusion:
Cobalt allergy is an immune-mediated hypersensitivity reaction to cobalt, a common metal found in various consumer products and industrial materials. While cobalt allergy is relatively rare, it can cause significant discomfort and impairment in affected individuals. Recognition of symptoms, accurate diagnosis through patch testing, and implementation of preventive measures are essential for managing cobalt allergy and reducing the risk of allergic reactions. Collaboration between patients, healthcare providers, and occupational safety professionals is critical for effective management and prevention of this allergy in both occupational and non-occupational settings. Ongoing research efforts aimed at understanding the underlying mechanisms of cobalt allergy and developing targeted therapies may further improve outcomes for individuals with this condition.
