Metal Allergy – Symptoms, Causes, Diagnosis & Treatment
Metal allergy, also known as metal hypersensitivity, is a condition characterized by an adverse reaction to metals commonly found in everyday objects, such as jewelry, clothing fasteners, or medical implants. While metal allergy is relatively rare, it can cause discomfort and potentially severe reactions in affected individuals. In this comprehensive overview, we will explore the symptoms, causes, diagnosis, and treatment options associated with metal allergy.
Symptoms of Metal Allergy:
Metal allergy symptoms can vary depending on the severity of the allergic reaction and the individual’s sensitivity to specific metals. Common symptoms include:
- Skin Irritation:
- Itching, redness, rash, or swelling at the site of contact with the metal.
- The rash may be localized or spread over a larger area of the skin.
- In severe cases, blisters or skin lesions may develop.
- Contact Dermatitis:
- Eczema:
- Eczema, or atopic dermatitis, is a chronic inflammatory skin condition that may be aggravated by metal allergy.
- Symptoms include dry, scaly patches of skin, intense itching, and sometimes oozing or crusting.
- Allergic Contact Dermatitis (ACD):
- ACD is a delayed hypersensitivity reaction that occurs when the immune system reacts to an allergen, such as metals like nickel, cobalt, or chromium.
- Symptoms may not appear until 24 to 48 hours after exposure and can persist for days or weeks.
- Localized Swelling or Inflammation:
- Swelling, tenderness, or warmth at the site of contact with the metal.
- Inflammation may affect joints, causing pain and stiffness, especially in individuals with metal implants or prostheses.
- Systemic Symptoms:
- In rare cases, metal allergy may cause systemic symptoms, such as generalized itching, hives, or even anaphylaxis, a severe and potentially life-threatening allergic reaction.
Causes of Metal Allergy:
Metal allergy occurs when the body’s immune system reacts abnormally to certain metals, triggering an allergic response. The exact cause of metal allergy is not fully understood, but several factors may contribute to its development:
- Genetic Predisposition:
- Genetic factors may play a role in determining an individual’s susceptibility to metal allergy.
- Certain genetic variations can increase the likelihood of developing allergic reactions to specific metals.
- Environmental Exposure:
- Prolonged or repeated exposure to metals through contact with jewelry, clothing fasteners, watches, or occupational exposure can sensitize the immune system and trigger allergic reactions.
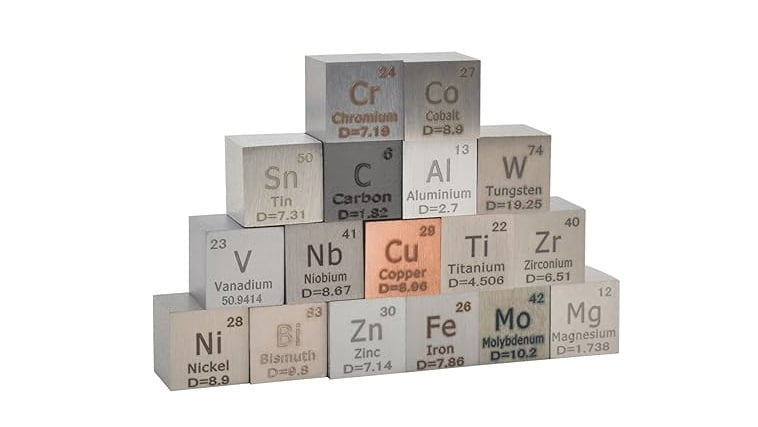
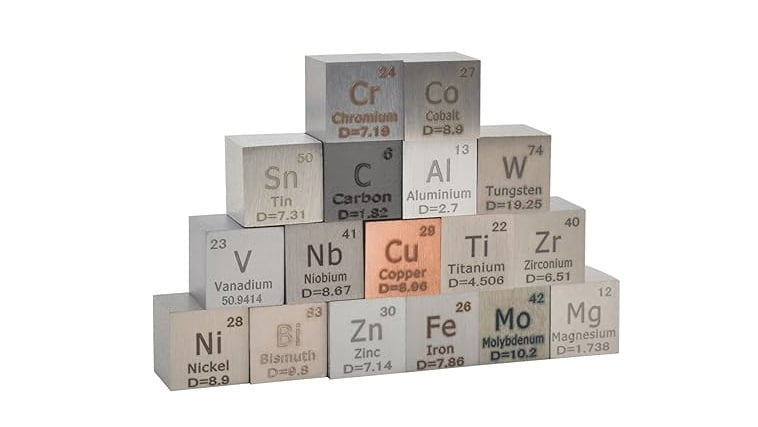
- Common allergenic metals include nickel, cobalt, chromium, and certain alloys used in metal objects.
- Skin Barrier Dysfunction:
- Skin conditions that compromise the integrity of the skin barrier, such as eczema or atopic dermatitis, may increase susceptibility to metal allergy.
- Damaged skin allows allergens to penetrate more easily, leading to sensitization and allergic reactions.
- Cross-Reactivity:
- Cross-reactivity occurs when the immune system reacts to structurally similar allergens.
- Metals with similar chemical properties may cross-react with each other, leading to allergic reactions in individuals sensitized to one metal.
- Implant Materials:
- Metal implants, such as orthopedic implants or dental materials, can occasionally trigger allergic reactions in susceptible individuals.
- Allergy to metals used in implants, such as nickel or cobalt, may lead to localized inflammation or systemic symptoms.
Diagnosis of Metal Allergy:
Diagnosing metal allergy typically involves a combination of medical history, physical examination, and specialized tests to identify the specific allergen responsible for the allergic reaction. Diagnostic steps may include:
- Clinical Evaluation:
- The healthcare provider will conduct a thorough medical history and physical examination, focusing on symptoms, potential exposures to metals, and previous allergic reactions.
- Patch Testing:
- Patch testing is the gold standard for diagnosing metal allergy. Small amounts of common allergenic metals, such as nickel, cobalt, or chromium, are applied to adhesive patches and placed on the patient’s back.
- After 48 hours, the patches are removed, and the skin is evaluated for signs of allergic reactions, such as redness, swelling, or rash.
- Blood Tests:
- Blood tests, such as specific IgE antibody tests or lymphocyte transformation tests (LTT), may be used to detect immune responses to specific metals.
- These tests are less commonly used than patch testing but may be helpful in certain situations, such as when patch testing is not feasible or inconclusive.
- Skin Prick Testing:
- Skin prick testing involves applying small amounts of allergenic substances to the skin and then pricking the skin to allow the allergen to enter.
- This test is more commonly used for diagnosing allergies to environmental allergens (e.g., pollen, pet dander) rather than metal allergy.
Treatment of Metal Allergy:
The treatment of metal allergy aims to manage symptoms, prevent further exposure to allergenic metals, and reduce the risk of allergic reactions. Treatment options may include:
- Avoidance of Allergenic Metals:
- The primary approach to managing metal allergy is to avoid contact with metals known to trigger allergic reactions.
- This may involve avoiding jewelry containing nickel, choosing hypoallergenic or inert metals for dental or medical implants, and using protective barriers (e.g., gloves) when handling metals in occupational settings.
- Topical Treatments:
- Topical corticosteroids or anti-inflammatory creams may be prescribed to relieve itching, redness, and inflammation associated with allergic contact dermatitis.
- Emollients or moisturizers can help soothe and hydrate the skin, reducing dryness and irritation.
- Oral Antihistamines:
- Oral antihistamines, such as cetirizine or loratadine, may be recommended to alleviate itching and reduce allergic symptoms.
- These medications block the action of histamine, a chemical released during allergic reactions.
- Systemic Corticosteroids:
- In severe cases of allergic contact dermatitis or eczema, short courses of oral corticosteroids may be prescribed to reduce inflammation and suppress the immune response.
- Systemic corticosteroids are typically used for short-term management due to the risk of side effects with prolonged use.
- Desensitization Therapy:
- Desensitization therapy, also known as allergen immunotherapy, involves exposing the immune system to gradually increasing doses of the allergen to induce tolerance and reduce allergic reactions.
- While desensitization therapy is commonly used for environmental allergies, its role in treating metal allergy is limited.
- Alternative Materials:
- In cases where metal allergy interferes with the use of medical implants or devices, alternative materials, such as titanium or ceramic, may be considered.
- These materials are less likely to trigger allergic reactions in sensitized individuals.
- Consultation with Dermatologist or Allergist:
- Referral to a dermatologist or allergist may be necessary for further evaluation and management, especially in cases of severe or persistent symptoms.
Prevention Strategies:
Preventing metal allergy involves minimizing exposure to allergenic metals and taking proactive measures to protect the skin. Key prevention strategies include:
- Choose Hypoallergenic Metals:
- Select jewelry and accessories made from hypoallergenic metals, such as titanium, stainless steel, or gold with a high karat content.
- Avoid jewelry containing nickel, cobalt, or other common allergenic metals.
- Protective Barriers:
- Use protective barriers, such as gloves or clothing liners, when handling metals in occupational or recreational settings.
- Apply clear nail polish or barrier creams to metal objects to create a protective barrier between the skin and the metal surface.
- Regular Skin Care:
- Maintain good skin hygiene by washing hands and exposed areas of skin with mild soap and water.
- Moisturize the skin regularly to prevent dryness and maintain the integrity of the skin barrier.
- Patch Testing Prior to Implantation:
- For individuals undergoing medical implantation procedures, consider patch testing for metal allergy prior to implantation.
- This can help identify potential sensitivities and inform the selection of implant materials less likely to trigger allergic reactions.
- Awareness of Occupational Hazards:
- Individuals working in industries with potential metal exposure, such as manufacturing, construction, or jewelry making, should be aware of occupational hazards and take appropriate precautions to minimize exposure.
Conclusion:
Metal allergy is a complex condition characterized by an abnormal immune response to certain metals, leading to allergic contact dermatitis and other allergic reactions. While relatively rare, metal allergy can cause significant discomfort and impair quality of life for affected individuals. Timely diagnosis, avoidance of allergenic metals, and appropriate treatment are essential for managing symptoms and preventing allergic reactions. Healthcare providers play a crucial role in educating patients about metal allergy, identifying potential triggers, and implementing preventive strategies to minimize exposure. By raising awareness and implementing proactive measures, individuals with metal allergy can effectively manage their condition and reduce the risk of allergic reactions.
Share this article
Metal allergy, also known as metal hypersensitivity, is a condition characterized by an adverse reaction to metals commonly found in everyday objects, such as jewelry, clothing fasteners, or medical implants. While metal allergy is relatively rare, it can cause discomfort and potentially severe reactions in affected individuals. In this comprehensive overview, we will explore the symptoms, causes, diagnosis, and treatment options associated with metal allergy.
Symptoms of Metal Allergy:
Metal allergy symptoms can vary depending on the severity of the allergic reaction and the individual’s sensitivity to specific metals. Common symptoms include:
- Skin Irritation:
- Itching, redness, rash, or swelling at the site of contact with the metal.
- The rash may be localized or spread over a larger area of the skin.
- In severe cases, blisters or skin lesions may develop.
- Contact Dermatitis:
- Eczema:
- Eczema, or atopic dermatitis, is a chronic inflammatory skin condition that may be aggravated by metal allergy.
- Symptoms include dry, scaly patches of skin, intense itching, and sometimes oozing or crusting.
- Allergic Contact Dermatitis (ACD):
- ACD is a delayed hypersensitivity reaction that occurs when the immune system reacts to an allergen, such as metals like nickel, cobalt, or chromium.
- Symptoms may not appear until 24 to 48 hours after exposure and can persist for days or weeks.
- Localized Swelling or Inflammation:
- Swelling, tenderness, or warmth at the site of contact with the metal.
- Inflammation may affect joints, causing pain and stiffness, especially in individuals with metal implants or prostheses.
- Systemic Symptoms:
- In rare cases, metal allergy may cause systemic symptoms, such as generalized itching, hives, or even anaphylaxis, a severe and potentially life-threatening allergic reaction.
Causes of Metal Allergy:
Metal allergy occurs when the body’s immune system reacts abnormally to certain metals, triggering an allergic response. The exact cause of metal allergy is not fully understood, but several factors may contribute to its development:
- Genetic Predisposition:
- Genetic factors may play a role in determining an individual’s susceptibility to metal allergy.
- Certain genetic variations can increase the likelihood of developing allergic reactions to specific metals.
- Environmental Exposure:
- Prolonged or repeated exposure to metals through contact with jewelry, clothing fasteners, watches, or occupational exposure can sensitize the immune system and trigger allergic reactions.
- Common allergenic metals include nickel, cobalt, chromium, and certain alloys used in metal objects.
- Skin Barrier Dysfunction:
- Skin conditions that compromise the integrity of the skin barrier, such as eczema or atopic dermatitis, may increase susceptibility to metal allergy.
- Damaged skin allows allergens to penetrate more easily, leading to sensitization and allergic reactions.
- Cross-Reactivity:
- Cross-reactivity occurs when the immune system reacts to structurally similar allergens.
- Metals with similar chemical properties may cross-react with each other, leading to allergic reactions in individuals sensitized to one metal.
- Implant Materials:
- Metal implants, such as orthopedic implants or dental materials, can occasionally trigger allergic reactions in susceptible individuals.
- Allergy to metals used in implants, such as nickel or cobalt, may lead to localized inflammation or systemic symptoms.
Diagnosis of Metal Allergy:
Diagnosing metal allergy typically involves a combination of medical history, physical examination, and specialized tests to identify the specific allergen responsible for the allergic reaction. Diagnostic steps may include:
- Clinical Evaluation:
- The healthcare provider will conduct a thorough medical history and physical examination, focusing on symptoms, potential exposures to metals, and previous allergic reactions.
- Patch Testing:
- Patch testing is the gold standard for diagnosing metal allergy. Small amounts of common allergenic metals, such as nickel, cobalt, or chromium, are applied to adhesive patches and placed on the patient’s back.
- After 48 hours, the patches are removed, and the skin is evaluated for signs of allergic reactions, such as redness, swelling, or rash.
- Blood Tests:
- Blood tests, such as specific IgE antibody tests or lymphocyte transformation tests (LTT), may be used to detect immune responses to specific metals.
- These tests are less commonly used than patch testing but may be helpful in certain situations, such as when patch testing is not feasible or inconclusive.
- Skin Prick Testing:
- Skin prick testing involves applying small amounts of allergenic substances to the skin and then pricking the skin to allow the allergen to enter.
- This test is more commonly used for diagnosing allergies to environmental allergens (e.g., pollen, pet dander) rather than metal allergy.
Treatment of Metal Allergy:
The treatment of metal allergy aims to manage symptoms, prevent further exposure to allergenic metals, and reduce the risk of allergic reactions. Treatment options may include:
- Avoidance of Allergenic Metals:
- The primary approach to managing metal allergy is to avoid contact with metals known to trigger allergic reactions.
- This may involve avoiding jewelry containing nickel, choosing hypoallergenic or inert metals for dental or medical implants, and using protective barriers (e.g., gloves) when handling metals in occupational settings.
- Topical Treatments:
- Topical corticosteroids or anti-inflammatory creams may be prescribed to relieve itching, redness, and inflammation associated with allergic contact dermatitis.
- Emollients or moisturizers can help soothe and hydrate the skin, reducing dryness and irritation.
- Oral Antihistamines:
- Oral antihistamines, such as cetirizine or loratadine, may be recommended to alleviate itching and reduce allergic symptoms.
- These medications block the action of histamine, a chemical released during allergic reactions.
- Systemic Corticosteroids:
- In severe cases of allergic contact dermatitis or eczema, short courses of oral corticosteroids may be prescribed to reduce inflammation and suppress the immune response.
- Systemic corticosteroids are typically used for short-term management due to the risk of side effects with prolonged use.
- Desensitization Therapy:
- Desensitization therapy, also known as allergen immunotherapy, involves exposing the immune system to gradually increasing doses of the allergen to induce tolerance and reduce allergic reactions.
- While desensitization therapy is commonly used for environmental allergies, its role in treating metal allergy is limited.
- Alternative Materials:
- In cases where metal allergy interferes with the use of medical implants or devices, alternative materials, such as titanium or ceramic, may be considered.
- These materials are less likely to trigger allergic reactions in sensitized individuals.
- Consultation with Dermatologist or Allergist:
- Referral to a dermatologist or allergist may be necessary for further evaluation and management, especially in cases of severe or persistent symptoms.
Prevention Strategies:
Preventing metal allergy involves minimizing exposure to allergenic metals and taking proactive measures to protect the skin. Key prevention strategies include:
- Choose Hypoallergenic Metals:
- Select jewelry and accessories made from hypoallergenic metals, such as titanium, stainless steel, or gold with a high karat content.
- Avoid jewelry containing nickel, cobalt, or other common allergenic metals.
- Protective Barriers:
- Use protective barriers, such as gloves or clothing liners, when handling metals in occupational or recreational settings.
- Apply clear nail polish or barrier creams to metal objects to create a protective barrier between the skin and the metal surface.
- Regular Skin Care:
- Maintain good skin hygiene by washing hands and exposed areas of skin with mild soap and water.
- Moisturize the skin regularly to prevent dryness and maintain the integrity of the skin barrier.
- Patch Testing Prior to Implantation:
- For individuals undergoing medical implantation procedures, consider patch testing for metal allergy prior to implantation.
- This can help identify potential sensitivities and inform the selection of implant materials less likely to trigger allergic reactions.
- Awareness of Occupational Hazards:
- Individuals working in industries with potential metal exposure, such as manufacturing, construction, or jewelry making, should be aware of occupational hazards and take appropriate precautions to minimize exposure.
Conclusion:
Metal allergy is a complex condition characterized by an abnormal immune response to certain metals, leading to allergic contact dermatitis and other allergic reactions. While relatively rare, metal allergy can cause significant discomfort and impair quality of life for affected individuals. Timely diagnosis, avoidance of allergenic metals, and appropriate treatment are essential for managing symptoms and preventing allergic reactions. Healthcare providers play a crucial role in educating patients about metal allergy, identifying potential triggers, and implementing preventive strategies to minimize exposure. By raising awareness and implementing proactive measures, individuals with metal allergy can effectively manage their condition and reduce the risk of allergic reactions.
